Comparison of stability and dosage of thermoplastic masks and vacuum bag for mediastinal cancer patients: a retrospective study
Introduction
The mediastinum cavity refers to structures locating at center of the thoracic cavity surrounded by loose connective tissue. This area contains various anatomical structures including heart and its surrounding vascular system, esophagus, trachea, phrenic nerve, cardiac nerve, thymus, and thoracic lymph nodes. In the early stage of mediastinal tumors, there are almost no symptoms. A few patients have chest tightness, chest pain, coughing and other uncomfortable feelings. As the tumor slowly grows, the tumor begins to compress the tissues and organs in the mediastinum, such as the trachea, heart, large blood vessels, esophagus, etc. Patient starts to suffered from more obvious symptoms, including dyspnea, wheezing, dysphagia, head and neck, and edema of the upper extremities. The treatment of mediastinal tumors must be based on the tumor type. In addition, tumor size, location, and aggressive status are also indicators for pre-treatment evaluation. Lung cancer has been the top three cancer death in our country for years, and esophageal cancer is also included in the top ten cancer death. Treatment strategies for both cancers include surgery, chemotherapy and radiotherapy.
Intensity modulated radiotherapy (IMRT) is the most important current radiotherapy treatment method. IMRT increases dose coverage and homogeneity of tumor region, and reduce dose to normal organs. However, the accuracy of IMRT treatment depends on daily position reproducibility. Fixation mold plays an important role in assisting reproduction of daily treatment position. While performing simulation before start of radiotherapy, selection of fixation mold type is important and depends on each hospital, compatible treatment couch, radiologists, and patient conditions.
For patients with mediastinal tumors, a vacuum bag was routinely used for simulated positioning at the beginning. However, patients with vacuum bag must have arms up, and the elevation angle of arm may vary everyday and will affect the position of the vacuum bag. Alternatively, we choose to use the thermoplastic masks, and found that it is more convenient to make and use, and there is no need to raise the arm like a vacuum bag, which is deeply favored by our team. Different fixed molds of the arm may cause different positional displacements every day, affecting the therapeutic dose distribution.
Analyzing daily setup errors could assist physician to design a proper treatment field to ensure daily cancer irradiation. The daily patient position compared with the simulation setup position is called a total setup error. The total setup error (TE) is a combination evaluation of systematic error (Σ) and random error (σ) of each treatment. The method for setup errors calculation has been described by el-Gayed et al. (1) and Gilbeau et al. (2). Setup errors were contributed by displacement of vertical direction, longitudinal, lateral, and rotation direction. Systematic error described the inter-patient error. Systematic error is calculated as the mean of all the displacements measured throughout the course of treatment. Random error describes inter-fraction error and calculated position displacement varies between day-to-day treatment during the treatment course. For each patient, the random error of a particular direction was assessed by subtraction of the systematic error from the daily displacement.
Σ represents means systematic error. σ is random error. The relationship among of total error (2), systematic (Σ) and random errors (σ) can be demonstrated as the formula:
In 2015, Navarro-Martin et al. evaluated setup displacement of thermoplastic masks (TMPs) and vacuum cushion system of patients with metastatic lung cancer. Their result showed that thermoplastic masks had significantly smaller setup displacement than vacuum cushion system (3). In 2017, Zhao et al. classified 60 thoracic tumor patients into four body types based on the body mass index (BMI): wasting group, moderate group, overweight group, and obese group. In the left-right direction (R-L), up-down (S-I) direction, and anterior-posterior (A-P) direction, the moderate group had the smallest displacement followed by the wasting group, overweight group, and finally the obese group. In the conclusion, the expansion margin of planning treatment volume (PTV) should be considered to be increased along with BMI value for thoracic tumor patients (4). Chen et al. (5). also verified that the positioning error of thermoplastic masks was better than vacuum bag with patient’s BMI <24 kg/m2. However, the study did not discuss the dosage of the two different mold types. Fixation ability of different mold has also been investigated at different tumor location. In 2018, Udayashankar et al. compared two fixation methods and non-immobilized technique with leg separator methods at pelvic external beam irradiation. A total of 65 patients received pelvic external beam radiation therapy. Thirty cases used non-immobilization with a leg separator, 21 cases used whole body vacuum bag and 14 cases used six-point aquaplas immobilization system. The results showed that the non-immobilized technique with leg separator had significantly better fixation ability than the thermoplastic mask and the whole body vacuum bag (6). According to the above results, different type of fixation mold could lead to various position errors. Patient characteristics and tumor location are also considerations in fixation mold selection. Therefore, our article aimed to understand the variation of positioning error and dosage distribution between thermoplastic chest mold and the vacuum bag.
This study mainly explored the positioning displacement of different fixed mold type in patients with mediastinum cancers. Data was analyzed to determine which fixed mold type provides better position reproducibility. The difference of dose received by the tumor tissue and the dose received by other normal tissues between the two different mold types were also calculated. We present the following article in accordance with the STROBE reporting checklist (available at https://tro.amegroups.com/article/view/10.21037/tro-21-25/rc).
Methods
Patient selection
This is a retrospective study. Truebeam® STx (Varian) system in Cathay General Hospital has been started to treat patient since January 2015. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by institutional review board of Cathay General Hospital in June 2020 (No. CGH P-109089). Thus, the study reviewed patients received radiotherapy in Cathay General Hospital between January 2015 and June 2020. Individual consent for this retrospective analysis was waived.
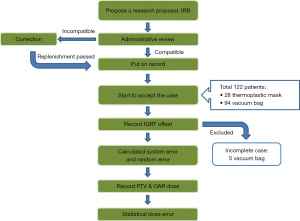
Patients received radiotherapy for mediastinum cancers were included. Since the setup error needs to consider all the treatment position displacement during the whole treatment course, those who did not finish whole course of treatment due to personal factors or expiration during treatment course were excluded. Patients who could not comply with orders or need assisted fixation other than vacuum bag or thermoplastic mold are excluded. The patients’ inclusion and exclusion were reviewed by one radiologist, one physicist and two radiotherapists. The flow diagram is shown in Figure 1.
The molds for chest fixation evaluation included thermoplastic mask (Klarity R462-1ST model) and vacuum bag (medicall R7515NL model) (Figure 2). After fixing shape of molds, computed tomography (CT) simulation was performed through GE Discovery CT590 RT. CT images were transmitted to the Eclipse Treatment Planning System (version 11.0, Varian Medical System, Los Angeles, CA, USA) for treatment planning.

Contouring and planning
The clinical treatment volume (CTV) and PTV were contoured by clinicians. Normal organs were contoured by physicists who have experience for more than 15 years. Prescription dose was 6,000 cGy for lung adenocarcinoma, 5,040 cGy for esophageal cancer and 4,500 cGy for lymph node region. Prescription dose for other mediastinum cancer types (thymic cancer, lymphoma… etc.) was ranged from 4,500 to 6,000 cGy. The conformality and dose limits of normal tissues were set according to RTOG 0412.
Radiotherapy was delivered through Varian TrueBeam STx linear accelerator. Image guided radiation therapy (IGRT) was performed before radiotherapy delivery for position confirmation. Cone beam CT was taken every treatment day. CT image registration was performed through auto matching function first and adjusted with manual control by radiotherapists. Tow radiotherapists with more than 5 years of experience repeatedly confirmed the position accuracy of the image.
Data measurement
Positioning displacement data was collected. Vertical direction was defined as front to back directions of patients. Longitudinal direction was defined as head to feet directions of patients. Lateral direction was defined as left to right direction of patients. Rotation direction was defined as head-to-foot rotation of patients. Systematic error and random error of each fixation mode was calculated. Analysis of position displacement data was performed to evaluate the correlation between position displacement and mold types (Figure 3).
All treatment plan doses were normalized to PTV 5,000 cGy for normal organ protection ability evaluation and comparison. Dose-volume histogram (DVH) was used to evaluate the dose distribution to PTV including maximum target volume dose (PTVmax), minimum target volume dose (PTVmin), average target volume dose (PTVavg) and organ at risk (OAR). Each data was collected and calculated for analysis.
Statistical analysis
All data was analyzed by independent-sample t-test with IBM® SPSS®, version 16 (SPSS IBM, Armonk, NY, USA), P value <0.05 is significantly (95% confidence interval).
Results
This article reviewed a total of 122 mediastinum patients with age between 30–90 years old. Twenty-eight people (19 males and 9 females) received thermoplastic mask fixation, and 94 people (70 males and 24 females) received vacuum bag fixation. Five patients were excluded from the study due to personal factors or expired and discontinued treatment. It was up to the clinical radiotherapist to decide. In the beginning, we used more vacuum bags. However, the skin marks on the upper mediastinum patient’s body will get stuck in the armpits, and the marks will be difficult to maintain after friction under the armpits or armpit hair. Later, we began to use the tumor location to distinguish. If the tumor is in the upper mediastinum, thermoplastic masks will be used for simulation; if the tumor is in the middle and lower mediastinum, vacuum bag will be used. Therefore, there are 89 patients with vacuum bags, thermoplastic masks 28 bits. The characteristics of patients were listed as Table 1. Systemic errors of thermoplastic mask and vacuum bag fixation were 1.40±1.41 and 2.44±2.44 mm in vertical direction (P=0.232), 1.70±1.70 and 4.14±4.14 mm in longitudinal direction (P=0.836), 1.18±1.18 and 2.05±2.05 mm in lateral direction (P=0.294), and 4.19±4.20 and 3.06±3.01 mm in rotational direction (P=0.697), respectively.
Table 1
| Patient characteristics | Thermoplastic mask | Vacuum bag |
|---|---|---|
| Patients numbers, n (%) | 28 (23.93) | 89 (76.07) |
| Gender, n (%) | ||
| Male | 19 (16.24) | 65 (55.56) |
| Female | 9 (7.69) | 24 (20.51) |
| Age, n (%) | ||
| >80 years | 2 (1.71) | 13 (11.11) |
| 71–80 years | 6 (5.13) | 20 (17.09) |
| 61–70 years | 7 (5.98) | 31 (26.50) |
| 50–60 years | 9 (7.69) | 22 (18.80) |
| <50 years | 4 (3.42) | 3 (2.56) |
| Tumor position (persons), n (%) | ||
| Lung | 13 (11.11) | 60 (51.28) |
| Esophageal | 12 (10.26) | 24 (20.51) |
| Others (thymoma, mediastinum, lymphoma) | 3 (2.56) | 5 (4.27) |
| Average PTV size (cm3) | 657.80±327.68 | 645.75±464.10 |
| Lung (R/L) | 662.12±365.98/653.48±203.48 | 601.16±367.23/690.33±568.83 |
| Esophageal | 868.90±272.24 | 711.47±262.10 |
| Others (thymoma, mediastinum, lymphoma) | 1,007.61±659.16 | 887.61±342.11 |
PTV, planning treatment volume; R/L, right/left.
Random errors of thermoplastic mask and vacuum bag fixation were 1.71±0.75 and 3.94 ± 3.22 mm in vertical direction (P<0.001), 2.43±1.30 and 4.60±6.11 mm in longitudinal direction (P<0.001), 2.86±2.34 and 3.22±2.55 mm in lateral direction (P=0.455), and 4.57±4.22 and 4.07±3.33 mm in rotational direction (P=0.673), respectively (Table 2).
Table 2
| Error (mm) | Axis | Thermoplastic mask | Vacuum bag | Cheng et al. (2014) | Halperin et al. (1998) | P value |
|---|---|---|---|---|---|---|
| Systematic error | Vrt | 1.40±1.41 | 2.44±2.44 | 2.70 | 5.40 | 0.23 |
| Lng | 1.70±1.70 | 4.14±4.14 | 2.30 | 3.60 | 0.84 | |
| Lat | 1.18±1.18 | 2.05±2.05 | 2.50 | 5.30 | 0.29 | |
| Rtn | 4.19±4.20 | 3.06±3.01 | N/A | N/A | 0.70 | |
| Random error | Vrt | 1.71±0.75 | 3.94±3.22 | 2.20 | N/A | <0.001* |
| Lng | 2.43±1.30 | 4.60±6.11 | 1.80 | N/A | <0.001* | |
| Lat | 2.86±2.34 | 3.22±2.55 | 1.30 | N/A | 0.46 | |
| Rtn | 4.57±4.22 | 4.07±3.33 | N/A | N/A | 0.67 |
*P<0.05. Vrt, vertical; Lng, longitudinal; Lat, lateral; Rtn, rotation.
For patients with lung cancers, 13 patients received thermoplastic mask fixation, and 60 patients received vacuum bag fixation. There was no significant difference of PTVmax, PTVmin, PTVavg, and dose to normal organs including trachea, esophagus, spinal cord, and right lung between two fixation mold types. However, thermoplastic masks had significantly lower Dmean (697.96 and 996.42 cGy, P=0.02), V20Gy (8.28 and 15.75 cGy, P=0.05), and V10Gy (23.70 and 32.43 cGy, P=0.03) of left lung and Dmean of heart (225.34 and 970.83 cGy, P=0.03) compared with vacuum bag (Table 3).
Table 3
| Organ | Thermoplastic mask (cGy) | Vacuum bag (cGy) | P value |
|---|---|---|---|
| PTVmax | 5,553.92 | 5,589.77 | 0.48 |
| PTVmin | 4,160.37 | 4,022.66 | 0.93 |
| PTVavg | 5,257.78 | 5,250.46 | 0.74 |
| Trachea Dmean | 3,023.83 | 2,922.73 | 0.39 |
| Esophagus Dmean | 3,227.41 | 2,598.47 | 0.11 |
| Heart Dmean | 225.34 | 970.83 | 0.03* |
| Spinal cord | |||
| Dmax | 3,422.78 | 3,453.87 | 0.61 |
| D1 | 3,217.70 | 3119.10 | 0.58 |
| Right lung | |||
| Dmean | 1,190.74 | 1071.42 | 0.91 |
| V20Gy (%) | 20.83 | 20.14 | 0.83 |
| V10Gy (%) | 33.88 | 37.08 | 0.71 |
| Left lung | |||
| Dmean | 697.96 | 996.42 | 0.02* |
| V20Gy (%) | 8.28 | 15.75 | 0.05* |
| V10Gy (%) | 23.70 | 32.43 | 0.03* |
*P<0.05. PTV, planning treatment volume.
For 36 patients with esophageal cancer, 12 patients received thermoplastic mask fixation and 24 patients received vacuum bag fixation. There is no significant difference of PTVmax, PTVmin, PTVavg, trachea, esophagus, spinal cord, heart, right lung (Dmean, V20Gy, V10Gy) and left lung (Dmean, V20Gy, V10Gy). However, thermoplastic mask fixation group had significantly lower Dmean of heart (P<0.001) (Table 4).
Table 4
| Organ | Thermoplastic mask (cGy) | vacuum bag (cGy) | P value |
|---|---|---|---|
| PTVmax | 5,587.99 | 5,587.65 | 0.95 |
| PTVmin | 4,689.76 | 4,264.51 | 0.31 |
| PTVavg | 5,275.94 | 5,253.22 | 0.19 |
| Trachea Dmean | 4,623.12 | 4,826.43 | 0.42 |
| Heart Dmean | 1,300.96 | 2,491.84 | <0.001* |
| Spinal cord | |||
| Dmax | 3,948.07 | 3,991.92 | 0.71 |
| D1 | 3,819.32 | 3,793.78 | 0.63 |
| Right lung | |||
| Dmean | 1,065.26 | 1,176.94 | 0.34 |
| V20Gy (%) | 17.48 | 19.31 | 0.54 |
| V10Gy (%) | 35.18 | 41.87 | 0.16 |
| Left lung | |||
| Dmean | 1,221.07 | 1,350.81 | 0.27 |
| V20Gy (%) | 23.40 | 23.58 | 0.96 |
| V10Gy (%) | 40.69 | 46.61 | 0.34 |
*P<0.05. PTV, planning treatment volume.
For patients with other cancers, 3 patients received thermoplastic mask fixation, and 5 patients received vacuum bag fixation. There is no significant difference of PTVmax, PTVmin, PTVavg, trachea, esophagus, spinal cord, heart, right lung (Dmean, V20Gy, V10Gy) and left lung (Dmean, V20Gy, V10Gy) (Table 5).
Table 5
| Organ | Thermoplastic mask (cGy) | Vacuum bag (cGy) | P value |
|---|---|---|---|
| PTVmax | 5,510.06 | 5,725.16 | 0.30 |
| PTVmin | 3,424.56 | 3,796.51 | 0.63 |
| PTVavg | 5,073.55 | 5,207.13 | 0.41 |
| Trachea Dmean | 3,395.06 | 2,873.93 | 0.46 |
| Esophagus Dmean | 3,525.90 | 3,529.71 | 0.99 |
| Heart Dmean | 946.36 | 1,085.94 | 0.79 |
| Spinal cord | |||
| Dmax | 3,698.27 | 3,631.54 | 0.71 |
| D1 | 3,483.96 | 3,402.19 | 0.64 |
| Right lung | |||
| Dmean | 1,453.19 | 1,088.17 | 0.36 |
| V20Gy (%) | 26.33 | 19.18 | 0.49 |
| V10Gy (%) | 44.96 | 34.60 | 0.35 |
| Left lung | |||
| Dmean | 1,571.49 | 1,348.27 | 0.67 |
| V20Gy (%) | 28.79 | 25.95 | 0.83 |
| V10Gy (%) | 47.72 | 44.94 | 0.77 |
PTV, planning treatment volume.
Discussion
According to our research, the systematic error of vacuum bag was 2.44±2.44 mm in Vertical direction and 2.05±2.05 mm in lateral direction. Both are smaller than 2.7 mm, and 2.5 mm in Cheng et al.’s study (7). Also, the results are smaller than 5.4 mm, 5.3 mm in Halperin et al.’s study (8). Multiple molding demands requirement at our department may explained the improvement of systemic error. While molding vacuum bag, the bilateral later border of vacuum bag was shaped be higher than patient’s body to ensure the reproducibility of the patient’s position.
IGRT was performed to confirm treatment position. After position was corrected according to image comparison, the shifting distance of vertical, longitudinal, lateral, and rotation was recorded and long three-axis cross marks were drawn on fixation mold and patient body. However, the systemic error of longitudinal direction was 4.14 mm which was inferior to the other two studies (7,8). In both Cheng and Halperin studies, a headrest was also set on vacuum bag to fix patient’s head and which can reproduce the longitudinal position more precisely. Instead, our unit made a groove in vacuum bag at patient’s head position. Depth and wide of head grooves varied and limited by shaping and amount of filling polystyrene which may decrease the precision of head and foot direction reproducibility. In previous studies, patient’s sole would be pressed against the mold to make feet groove during mold shaping for repositioning and reduce the displacement of the longitudinal direction. However, the length of vacuum bags in our department can cover more than half of adult’s body but not whole body. The vacuum bags can only cover from head and down to hip. Since patient’s sole could not be used for longitudinal fixation in our vacuum bag, longitudinal systematic displacement of our study could be larger than the references.
The systematic error values of thermoplastic mask in this article were 1.40±1.41, 1.70±1.70, 1.18±1.18 mm in vertical, longitudinal, lateral direction, respectively. These values were also smaller than the Cheng’s study. Random errors are generally better than the values in the literatures. Thermoplastic mask was pressed down from the top of the face to plate to fix patient after patient lying stable on a fixed plate and headrest. After the thermoplastic mask cooled, patient’s eyebrows and eyes were drawn on the mask. IGRT was performed before treatment to confirm the correct treatment position. After position confirmed, treatment center marks were redrawn on thermoplastic mask and recorded the couch coordinate for subsequent alignment purposes. Thermoplastic mask fixation can be aided by rechecking position of patient’s eyes, eyebrows, bridge of nose, and ear holes. Thermoplastic mask also can verify the position of top of patient’s and make sure that patient is lying in the correct position.
Compared with the thermoplastic mask, vacuum bag fixation utilizes head-shaped groove to determine longitudinal position. However, daily head position may decrease due to spherical shape of head and thereby affecting the patient’s head and feet direction. Lateral and vertical position may be affected by breathing condition. Any condition including disease associated discomfort and pain may decrease stability of breathing cycle and increase the systemic error of lateral and vertical directions.
The results showed that in lung cancer patient group, there was no significant difference of PTVmax, PTVmin, PTVavg, trachea (Dmean), esophagus (Dmean), spinal cord (Dmax, D1 <4,500 cGy), right lung (Dmean, V20Gy, V10Gy) between thermoplastic mask and vacuum bag but significant lower heart (Dmean) and Dmean, V20Gy, V10Gy of left lung in thermoplastic fixation. Our study retrospectively reviewed 13 patients with thermoplastic masks. Ten patients had tumors at right lung and 3 patients had tumors at the upper left lung. The number of patients with tumors at left lung is quite small and leads to the low average dose to left lung and heart.
There are some limitations of our study. The number of patients with thermoplastic masks fixation is small. Further subsequent experiments with large patient number is needed to confirm whether the rotation displacement can be corrected. Secondly, all mediastinal patients have been included, and the BMI has not yet been classified. We suggest BMI will be classified to determine the positioning errors of different BMIs in the mediastinum.
Thirdly, because our department only used thermoplastic masks and vacuum bags, it is recommended to introduce several different positioning molds for comparison, such as α-cradle or other molds can achieve the same fixing effect.
Conclusions
This study explored comparison of position stability and dosage of different fixation molds in patients with cancers in mediastinum. Both two fixation molds are good fixation choices for clinical practice and no significant difference in dosage distribution between two fixation mold types. Thermoplastic mask provided better head to feet direction position reproducibility than vacuum bag. When choosing fixation mold type for patients with cancers in mediastinum, Thermoplastic masks can be considered and extending a long midline can assist body rotation position correction.
Acknowledgments
We would like to thank Medical Research Center of Cathay General Hospital for the statistical consultation.
Funding: This work was supported by the Cathay General Hospital.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tro.amegroups.com/article/view/10.21037/tro-21-25/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tro.amegroups.com/article/view/10.21037/tro-21-25/coif). HCC serves as a technologist of the Department of Radiation Oncology, Cathay General Hospital from March 2010 to November 2016. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional review board of Cathay General Hospital (No. CGH P-109089) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- el-Gayed AA, Bel A, Vijlbrief R, et al. Time trend of patient setup deviations during pelvic irradiation using electronic portal imaging. Radiother Oncol 1993;26:162-71. [Crossref] [PubMed]
- Gilbeau L, Octave-Prignot M, Loncol T, et al. Comparison of setup accuracy of three different thermoplastic masks for the treatment of brain and head and neck tumors. Radiother Oncol 2001;58:155-62. [Crossref] [PubMed]
- Navarro-Martin A, Cacicedo J, Leaman O, et al. Comparative analysis of thermoplastic masks versus vacuum cushions in stereotactic body radiotherapy. Radiat Oncol 2015;10:176. [Crossref] [PubMed]
- Zhao J, Zhang M, Zhai F, et al. Setup errors in radiation therapy for thoracic tumor patients of different body mass index. J Appl Clin Med Phys 2018;19:27-31. [Crossref] [PubMed]
- Chen G, Dong B, Shan G, et al. Choice of immobilization of stereotactic body radiotherapy in lung tumor patient by BMI. BMC Cancer 2019;19:583. [Crossref] [PubMed]
- Udayashankar AH, Noorjahan S, Srikantia N, et al. Immobilization versus no immobilization for pelvic external beam radiotherapy. Rep Pract Oncol Radiother 2018;23:233-41. [Crossref] [PubMed]
- Cheng KF, Wu VW. Comparison of the effectiveness of different immobilization systems in different body regions using daily megavoltage CT in helical tomotherapy. Br J Radiol 2014;87:20130494. [Crossref] [PubMed]
- Halperin R, Roa W, Field M, Hanson J, Murray B. Setup reproducibility in radiation therapy for lung cancer: a comparison between T-bar and expanded foam immobilization devices. Int J Radiat Oncol Biol Phys 1999;43:211-6. [Crossref] [PubMed]
Cite this article as: Lin CW, Yu PC, Nien HH, Chang HC, Wu CJ. Comparison of stability and dosage of thermoplastic masks and vacuum bag for mediastinal cancer patients: a retrospective study. Ther Radiol Oncol 2022;6:6.