Adjuvant radiotherapy for sebaceous carcinoma of the eyelid after orbital exenteration
Introduction
Sebaceous carcinoma is a comparatively rare form of cancer, wherein the involvement of orbital and adjacent critical structures is often noted. An optimal treatment option for sebaceous carcinoma of the orbital region is surgical excision. Subsequently, postoperative radiotherapy is suggested for those displaying adverse pathological features such as lymphovascular permeation, perineural invasion, and involved margins. Because tumor recurrence in this region could compromise both the cosmetic outcome and functional preservation, combining the treatment modalities mentioned above to minimize local recurrence is paramount. Here, we present a case of sebaceous carcinoma of the eyelid that was treated with recurrent surgeries and adjuvant radiotherapy following the last surgery. The patient has been followed up at our clinic for 15 months after radiotherapy with no evidence of locoregional recurrence. We believe that this successful experience demonstrates the feasibility of this combined treatment approach.
Case presentation
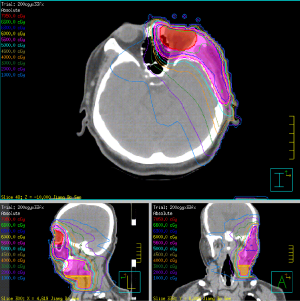
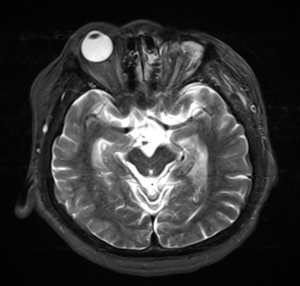
We present the case of a 54-year-old male with an underlying disease of type II diabetes mellitus. His medical history includes complaints of chronic ulceration and erosion over the left upper eyelid for 5 years, accompanied by visual disturbances, swelling, and pain, for which he had first approached our rheumatology clinic in 2010. A blood examination, including complete blood count and differential count, erythrocyte sedimentation rate, glutamic oxaloacetic transaminase, glutamic pyruvic transaminase, creatinine, antinuclear antibody, and HLA-B27, was conducted, ruling out autoimmune diseases. Subsequently, he was referred to the ophthalmology clinic for further examination and treatment. Besides visual disturbances, severe blepharitis, skin erosion, trichiasis, and corneal neovascularization were noted. Visual acuity tests were 0.3 for the right eye and 0.1 for the left eye. An incisional biopsy of the left upper eyelid conducted on June 08, 2011, revealed sebaceous carcinoma. Clinically, the disease was staged as cT1N0Mx according to the American Joint Committee on Cancer 7th edition (AJCC 7th). Therefore, 2 days later, lesion excision combined with semicircular flap reconstruction as well as left lower eyelid biopsy was conducted. The pathology report revealed the following: (I) residual sebaceous carcinoma with free section margins of the upper eyelid, with the closest margin of approximately 1 mm at the nasal side; and (II) the lower eyelid section exhibiting sebaceous carcinoma among the marked inflammatory background. The disease was pathologically staged as pT1cN0Mx, according to the AJCC 7th. Thereafter, the patient was followed up at the ophthalmology clinic no symptoms noted for years. In January 2015, the patient returned to the ophthalmology clinic with a complaint of progressive erythema over the left eyelid that he had been experiencing for months. Visual acuity test was 0.1 for the left eye. We scheduled a biopsy of the left upper, lower eyelids, and conjunctiva to rule out recurrent malignancy; however, the planned procedure was canceled by the patient. Thereafter, the patient revisited our ophthalmology clinic in June 2016, during which we observed diffuse inflammation and erosion of the left eyelids and the Meibomian gland as well as severe blepharitis, pannus, and symblepharon. Moreover, severe deterioration of the left eye was noted, with visual acuity determined as no light perception and limited extraocular movement. According to the patient’s statement, the deterioration of the left eye function has been observed for over a year. On June 27, 2016, an incisional biopsy of the left eyelids was finally conducted; the pathology report revealed recurrent sebaceous carcinoma with the deep margin free from tumor cells but the peripheral margin displaying crushed tumor cells. Based on the clinical picture, the recurrent disease was staged as rcT3bN0Mx, according to the AJCC 7th. Considering the irreversibility of the left eye function, organ preservation was of little significance to the patient himself; instead, he preferred a treatment that would minimize the chances of future recurrences. Accordingly, the patient was suggested orbital exenteration combined with postoperative radiotherapy to enhance the local control of the disease. In addition, definitive radiotherapy as another treatment option was suggested to the patient, although better local control might be achieved with radical surgery followed by adjuvant radiotherapy. Moreover, although neoadjuvant chemotherapy was suggested to the patient, it was not included in the treatment plan owing to his preference. Nonetheless, the patient desired to review the options before deciding on a treatment plan; he was lost to follow-up until 6 months later in January 2017 and had sought a second opinion during this period. The patient decided upon orbital exenteration combined with postoperative radiotherapy as the treatment plan on April 06, 2017. Accordingly, a contrast-enhanced magnetic resonance imaging (MRI) of the orbit conducted for tumor survey revealed increased T2-weighted imaging intensity and enhancement at the left-side eyelid (Figure 1). A 18F-FDG positron emission tomography (PET) scan conducted for distant metastasis assessment revealed negative findings. According to the AJCC 7th, the tumor was clinically staged as rcT3bN0M0, rc-stage IIIA. On April 24, 2017, surgical intervention as orbital exenteration of the left eye was performed (Figure 2); the pathology report revealed sebaceous carcinoma with pagetoid epidermal extension, with no lymphovascular permeation, free peripheral epidermal margins, an uninvaded eyeball, and a close deep soft tissue margin less than 1 mm. Pathologically, the disease was staged as rpT3bcN0M0, rp-stage IIIA, according to the AJCC 7th. On May 25, 2017, the patient was referred to our radiation oncology clinic for the evaluation of postoperative radiotherapy. Although the pathological report revealed an uninvaded eyeball, owing to concerns of the close deep soft tissue margin, advanced T stage, and aggressive nature of this disease, treatment with adjuvant radiotherapy was administered following discussion with the patient. Computed tomography (CT) simulation was completed on June 01, 2017. The patient was simulated in a supine position, with his head on a headrest device and a thermoplastic mask covering his head. CT simulation (GE Discovery CT 590 RT) was used to obtain imaging data for target delineation and treatment planning. Clinical target volumes (CTVs) and dose prescriptions were as follows: CTV-1, 6,600 cGy in 33 fractions administered to the tumor bed; CTV-2, 6,000 cGy in 33 fractions administered to the preauricular nodes and to the left neck level Ib–II; CTV-3, 5,600 cGy in 33 fractions administered to the left neck level III–Va. Planning target volumes were created using CTVs along with 5-mm expansion to account for daily motion and set-up errors, and the maximum (Dmax) and mean (Dmean) doses for the organs-at-risks were as follows: the right eyeball, Dmean <400 cGy and Dmax <700 cGy; the right lens, Dmean <300 cGy and Dmax <400 cGy; the right optic nerve, Dmax <2,500 cGy; the right parotid gland, Dmean <800 cGy and Dmax <1,000 cGy; and the vestibulocochlear nerve, Dmax <3,500 cGy (Figure 3). Intensity-modulated beams were planned using Pinnacle treatment planning system version 9.10. Image verification before treatment was conducted using plain films obtained from anteroposterior and lateral views. The treatment was administered using a Varian 21EX linear accelerator. From July 11 to August 30, 2017, radiotherapy was administered to the patient. During the patient’s treatment course and follow-ups after the completion of radiotherapy, acute toxicities, including grade 2 pruritus, dermatitis, and grade 1 mucositis, were observed but controlled well using topical agents. At the 3-month follow-up, an MRI of the orbit revealed no evidence of recurrence (Figure 4). To date, the patient was followed up at our clinic for 15 months since radiotherapy, and the last follow-up revealed the stable condition of the treated area with no evidence of locoregional recurrence (Figure 5). Overall, no late side effects were noted during the 15-month follow-up period.



Discussion
Sebaceous carcinoma of the eyelid is known for its high local recurrence rate. Watanabe et al observed local recurrences, particularly in diseases exceeding stage T3a (1). However, we describe a patient who experienced a local recurrence 4 years after the first excision. Fortunately, our patient experienced neither regional nodal metastases nor distant spread according to 18F-FDG PET-CT at the time of recurrence, allowing us to resolve his recurrent disease with reoperation followed by adjuvant radiotherapy (2,3).
Hata et al. reported adjuvant radiotherapy doses (range, 50–61 Gy) in 25–33 fractions to the tumor bed in patients with positive or close surgical margins and 44–50.6 Gy to the cervical lymph nodes as prophylactic irradiation, although it remains unclear whether prophylactic irradiation improves locoregional control or survival outcomes (4). Hashimoto et al. reported that among 21 patients with lymph node metastasis in a series of 268 eyelid carcinomas, the occurrence of regional recurrence in patients who received adjuvant radiotherapy (14.3%) was lower than that in patients without adjuvant radiotherapy (57.1%) (5). Therefore, considering the aggressive nature of this disease and the high likelihood of nodal spread, we decided to administer all-inclusive irradiation to the tumor bed and the lymphatic areas of the left neck.
Although no recognized consensus exists regarding systemic chemotherapy in the management of sebaceous carcinoma of the eyelid, Kaliki et al. used neoadjuvant chemotherapy to enable minimally invasive eyelid surgery or avoid orbital exenteration and observed, at least, moderate response (defined as 50–75% reduction in the eyelid tumor size) in those cases (6). In our case, systemic chemotherapy, although suggested to the patient, was not included in the multimodality treatment strategy owing to his preference. Therefore, the radical treatment approach of orbital exenteration followed by adjuvant radiotherapy was performed.
Conclusions
In summary, this report reveals that the combination of a radical surgical approach and postoperative adjuvant radiotherapy could be a satisfactory and safe treatment approach in patients with recurrent locally advanced sebaceous carcinoma of the eyelid.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Watanabe A, Sun MT, Pirbhai A, et al. Sebaceous carcinoma in Japanese patients: clinical presentation, staging and outcomes. Br J Ophthalmol 2013;97:1459-63. [Crossref] [PubMed]
- Krishna SM, Finger PT, Chin K, et al. 18-FDG PET/CT staging of ocular sebaceous cell carcinoma. Graefes Arch Clin Exp Ophthalmol 2007;245:759-60. [Crossref] [PubMed]
- Kumabe A, Kawase T, Miura K, et al. Sebaceous carcinoma of the parotid gland: F-18 FDG PET/CT findings. Clin Nucl Med 2010;35:260-2. [Crossref] [PubMed]
- Hata M, Koike I, Omura M, et al. Noninvasive and curative radiation therapy for sebaceous carcinoma of the eyelid. Int J Radiat Oncol Biol Phys 2012;82:605-11. [Crossref] [PubMed]
- Hashimoto K, Yasumatsu R, Toh S, et al. Patterns of lymphatic spread and the management of eyelid carcinomas. Auris Nasus Larynx 2016;43:666-71. [Crossref] [PubMed]
- Kaliki S, Ayyar A, Nair AG, et al. Neoadjuvant Systemic Chemotherapy in the Management of Extensive Eyelid Sebaceous Gland Carcinoma: A study of 10 Cases. Ophthal Plast Reconstr Surg 2016;32:35-9. [Crossref] [PubMed]
Cite this article as: Huang YH, Chang TH, Chou TW, Liu MT, Pi CP, Huang CC, Hung LC, Lin JB. Adjuvant radiotherapy for sebaceous carcinoma of the eyelid after orbital exenteration. Ther Radiol Oncol 2019;3:21.