Treating papillary tumors of the breast—role of adjuvant treatment—a narrative review
Introduction
Papillary tumours of the breast are rare and heterogenous lesions of the breast accounts for less than 3% of all breast tumours (1). The 5th edition of World Health Organization (WHO) Classification of Breast Tumors (2), describes these tumours in detail ranging from benign intraductal papilloma to invasive papillary carcinoma (IPC). Most of these lesions are benign and only a minority show atypical behaviour or malignant characteristics. The majority of them have overlapping histological features with low concordance in their diagnosis (3). Also, there are no pinpoint clinic-radiological characteristics attributable to these lesions. They can be central or peripheral in location and are not always readily detectable on radiological imaging. Thus they have an uncertain clinical behaviour. It is not uncommon for these lesions to be diagnosed in asymptomatic females and/or on screening.
Usually, there is a 1.5–2 times higher incidence of future breast carcinoma as compared to the general population, in women with benign duct papilloma which increases to 4.3 times if associated with atypia (4). There is a dearth of randomized clinical data available for this disease entity. The majority of the recommendations come from case series or retrospective studies. To treat or not, to prescribe any adjuvant treatment or not are some debatable questions because of mixed results from the literature. Here, I have tried to review the role of adjuvant treatment if any, in these lesions. I present this article in accordance with the Narrative Review reporting checklist (available at https://tro.amegroups.com/article/view/10.21037/tro-22-19/rc).
Methods
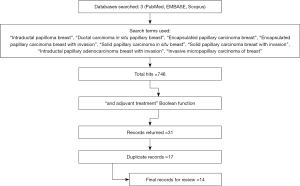
Recent articles on the topic covering papillary lesions of the breast were retrieved from databases including PubMed, EMBASE, Scopus. Due to the rarity of the disease only retrospective studies, case series or review articles were available for literature review. To be specific as for the use of adjuvant treatment is concerned only the literature published between January 2015 till August 2021 in English language only was reviewed (Table 1).
Table 1
| Items | Specification |
|---|---|
| Date of search | 09 September, 2021 |
| Databases and other sources searched | PubMed, EMBASE, Scopus |
| Search terms used | “Intraductal papilloma breast”, “Ductal carcinoma in situ papillary breast”, “Encapsulated papillary carcinoma breast”, “Encapsulated papillary carcinoma breast with invasion”, “Solid papillary carcinoma in situ breast”, “Solid papillary carcinoma breast with invasion”, “Intraductal papillary adenocarcinoma breast with invasion”, “Invasive micropapillary carcinoma of breast” |
| Timeframe | January 2015–August 2021 |
| Inclusion and exclusion criteria | Inclusion: (I) English language studies; (II) case series and review articles |
| Exclusion: non-English | |
| Selection process | Mohsin Khan did the study selection and review |
Results
The search strategy included the following terms: “Intraductal papilloma breast”, “Ductal carcinoma in situ papillary breast”, “Encapsulated papillary carcinoma breast”, “Encapsulated papillary carcinoma breast with invasion”, “Solid papillary carcinoma in situ breast”, “Solid papillary carcinoma breast with invasion”, “Intraductal papillary adenocarcinoma breast with invasion”, “Invasive micropapillary carcinoma of breast”. Initial search on 9 September, 2021 resulted in 746 hits with above mentioned terms. However, when search results were narrowed down to “and adjuvant treatment” Boolean function, 31 records were returned. Out of these 31 records 17 overlapping records were found. Thus for final analysis, data from 14 records was reviewed (Figure 1).
Discussion
Benign breast papilloma
Benign lesions include solitary intraductal papilloma and intraductal papillomatosis. An international multicentre review of the malignancy rates of excised papillomatous lesions of the breast (4), found that the upgrade rates from benign core needle biopsy to malignancy are somewhere near 14.4% and out of these 3.7% had invasive disease. Another retrospective review by Moynihan et al. (5) revealed that patients with benign papilloma without atypia on core biopsy have a low risk of upgrade to malignancy, with upgrade rates to malignancy of 2.4%. With this background, it can be argued that with such low rates of upgradation these lesions can safely be followed with the watch and wait for policy. This is particularly more relevant in women less than 35 years of age group where no upgradation rates to invasive disease were found. However, authors from the International Conference on lesions of uncertain malignant potential in the breast (B3 Lesions) recommended that even in such lesions underestimation of the stage can occur with core needle biopsy, warranting the use of a vacuum-assisted biopsy (VAB) in such lesions if wait and watch policy is to be adopted (6).
Atypical lesions
Upgrade rates after surgical excision of the papillary lesion with atypia can be as high as 28% (7). Even if these lesions are diagnosed on VAB there is a high possibility of them being malignant and therefore, surgical excision is warranted (8)
There is no role of any form of adjuvant treatment in benign papillary lesions even when associated with atypia provided they have been adequately excised. Some case reports in the literature do suggest the role of adjuvant treatment (9). However, they are single case reports especially describing multiple recurrent benign lesions. This may be due to invasive lesions masquerading as a benign prototype.
In-situ and invasive papillary lesions
Important prognosticators
Size of lesion
Usually these lesions present with small-sized tumours. Hassan et al. (10), in a recent analysis on the clinical presentations of these lesions reported that the median tumour size was 2 cm (range, 0.2 to 6 cm). When individual tumours were stratified according to size pure in situ lesions had a median size of 1.9 cm (1.2 to 4 cm), and those with associated invasion had the largest median size, 2.4 cm (0.2 to 6 cm). In a population-based study, Zheng et al. (11) reported that the majority of the invasive papillary lesions presented with smaller-sized tumours as compared to their ductal counterparts.
Nodal status
Although less common, axillary lymph node metastasis has been noted even without frank invasion. However, in Surveillance, Epidemiology, and End Results (SEER) database analysis Mogal et al. (12) reported that out of all the patients who had axillary nodal status available only 5.5% had tumour involvement. Concerning invasive disease, another SEER data reported that the rate of lymph nodal involvement at diagnosis was lower in invasive papillary cancers (11.6%) (11). This rate was significantly less when compared to the patients with invasive ductal carcinoma (IDC).
Distant metastasis
Sedano et al. (13) on presenting their literature review reported the rate of distant metastasis to be around 1.9%. This was in agreement with the less than 1% rate for distant metastasis reported in the SEER data (12).
Grade (Gr)
Majority of the patients present with Gr 1 or 2 diseases. In the SEER report, nearly 81.9% of the patients presented with Gr 1 or 2 disease (12). Similarly for invasive disease, 73.8% of the patients had Gr 1 or 2 lesions in comparison to invasive ductal disease where 34.1% presented with Gr 3 disease.
Hormone receptor and HER 2 neu status
More than 90% of the in situ lesions express estrogen receptor/progesterone receptor (ER and/or PR) (12). Their invasive counterparts also strongly express ER and or PR (14). Occasionally, these may be human epidermal growth factor receptor 2 (Her2Neu) positive (14,15).
Ki67 and p53
These lesions have been shown to possess a low Ki67 index (less than 20) and p53 status (less than 10%) in more than two third of the patient’s data as reported by Zhang et al. from a major Chinese cancer centre (14).
Thus, to summarize, in-situ as well as invasive papillary lesions usually have favourable prognosticators with small tumour size presentation, low nodal burden, well to moderately differentiated lesions, hormone receptor-positive with low proliferative indices. With this background, we now discuss the adjuvant treatment for these lesions.
Role of radiotherapy
Mogal et al. (12) reported that the use of radiation post-lumpectomy improved survival as compared to the use of surgery alone. In their analysis of around 2,649 patients from the SEER data having a diagnosis of intracystic papillary carcinoma, they found a statistically significant improvement in survival with P<0.0001 for patients who received post-lumpectomy radiation. This stands true even on multivariate analysis. However, the authors did not find any significant difference in survival in patients who received either a lumpectomy or mastectomy.
Fakhreddine et al. (16) found that among 10,485 patients with invasive papillary breast carcinoma at a median follow up of 56 months, patients treated with lumpectomy combined with radiation had a superior mean overall survival as compared to those who received mastectomy alone or lumpectomy alone. Improved overall survival also correlated with lower histologic grade, lower T stage and younger age. They concluded that lumpectomy alone is not an appropriate treatment for all early-stage patients with IPC and that radiation therapy (RT) needs to be a component of adjuvant treatment.
In a recent analysis by Huang et al. (15) the authors while investigating the clinic-pathological characteristics between IPC and IDC of breast and their prognosis, revealed that elderly patients, advanced stage and no RT use were associated with poor prognosis.
Thus, post-lumpectomy RT should be offered to all the patients of in-situ and IPC patients even in the presence of favourable prognosticators.
Role of hormonal therapy
As discussed earlier majority of the papillary tumours of the breast are hormone receptor-positive (>80%). Thus it is logical to prescribe hormonal agents in adjuvant settings. Zhang et al. (14) reported in their experience from a major Chinese cancer centre, that 86.5% of the patients with intra-cystic papillary carcinoma were hormone receptor-positive and nearly 84.7% received hormonal therapy. In the SEER database study too (12), 90.2% had hormone receptor-positive disease. Adjuvant hormonal therapy was frequently administered, though they did not provide exact numbers, however, they concluded that the benefit of adjuvant hormonal therapy in patients receiving radiotherapy or not was likely similar.
In another SEER investigative data in invasive papillary lesions (11), higher rates of ER/PR positivity were found in IPC tumours as compared to IDC (P<0.001). This accounted for a better prognosticator in IPC tumours and benefit from hormonal therapy. In a recent trial by Huang et al. (15) IPC tumours were more likely to be hormone receptor-positive as compared to IDC tumours. The use of hormonal therapy in such tumours was found to be prognostic for 5-year overall survival on univariate analysis. However, such a result was not duplicated on multivariate analysis.
With this background, hormonal therapy should be considered as an adjuvant in hormone receptor-positive papillary tumours whether in-situ lesion post-surgery or IPCs.
Role of chemotherapy
As discussed earlier, the majority of the papillary tumours have favourable prognosticators even if associated with invasive components. Early T stage, lymph nodal negative, low grade, hormone-receptor-positive disease are the hallmarks of these lesions. With these ‘ideal’ findings it is imperative to hypothesise that the use of systemic chemotherapy should be very limited. Indeed, Turashvili et al. (17) while reporting the data on 21-gene recurrence score (RS) in these special histologic subtypes of invasive breast carcinoma noted that papillary carcinomas usually have a low recurrence score (<18). The benefit of chemotherapy in patients with breast carcinoma of low RS is estimated to be too small to outweigh the risks of side effects.
National Cancer Comprehensive Network (NCCN) guidelines recommend the use of adjuvant hormonal therapy alone, even in lesions with T3 status provided they are node-negative or with microscopic nodal positivity (pN0 or pNi+). However, for node-positive, i.e., pN+ with at least ≥ ipsilateral metastases >2 mm, the use of adjuvant chemotherapy in addition to adjuvant hormonal therapy can be considered (18).
Huang et al. (15) reported that stage for stage, the utilization of chemotherapy was less marked in IPCs as compared to IDCs. Adjuvant chemotherapy was used in only 16.1% of the patients diagnosed with IPC as compared to 44.9% of patients with IDC histology. 83% of patients with IDC stage 3 received chemotherapy whereas, only 45.3% with IPC received chemotherapy. Even with this less aggressive treatment, there was no significant overall survival difference between these two histo-pathologies. Thus, with the presence of papillary histology, the treatment can be de-escalated in accordance with the NCCN guidelines.
Conclusions
After the literature search and based on the results from the above-mentioned trials it can be concluded as of now that (I) there is no role of any form of adjuvant treatment in benign papillary lesions even if they are multiple or associated with atypia; (II) adjuvant radiotherapy should be offered to all in-situ lesions including encapsulated papillary carcinomas and solid papillary carcinomas with or without hormonal therapy based on hormonal receptor status; and (III) post resection adjuvant radiation with or without hormonal therapy should be offered in IPCs with systemic chemotherapy reserved in lymph node-positive diseases only.
However, more prospective and large-scale retrospective studies are needed in the future to further validate our conclusions and to figure out the influence of loco-regional treatments as well as systemic treatment on long-term survival.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The author has completed the Narrative Review reporting checklist. Available at https://tro.amegroups.com/article/view/10.21037/tro-22-19/rc
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at https://tro.amegroups.com/article/view/10.21037/tro-22-19/coif). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lara Nuñez D, Candanedo González F, Chapa Ibargüengoitia M, et al. Papillary lesions of the breast: a review. Breast Cancer Management 2020; [Crossref]
- WHO Classification of Tumours Editorial Board. Breast tumours. WHO classification of tumour series, 5th ed., vol. 2. Lyon (France): International Agency for Research on Cancer; 2019.
- Tay TKY, Tan PH. Papillary neoplasms of the breast-reviewing the spectrum. Mod Pathol 2021;34:1044-61. [Crossref] [PubMed]
- Foley NM, Racz JM, Al-Hilli Z, et al. An International Multicenter Review of the Malignancy Rate of Excised Papillomatous Breast Lesions. Ann Surg Oncol 2015;22:S385-90. [Crossref] [PubMed]
- Moynihan A, Quinn EM, Smith CS, et al. Benign breast papilloma: Is surgical excision necessary? Breast J 2020;26:705-10. [Crossref] [PubMed]
- Rageth CJ, O'Flynn EAM, Pinker K, et al. Second International Consensus Conference on lesions of uncertain malignant potential in the breast (B3 lesions). Breast Cancer Res Treat 2019;174:279-96. [Crossref] [PubMed]
- Bekes I, deGregorio A, deWaal A, et al. Review on current treatment options for lesions of uncertain malignant potential (B3 lesions) of the breast: do B3 papillary lesions need to be removed in any case by open surgery? Arch Gynecol Obstet 2019;300:481-4. [Crossref] [PubMed]
- Wang ZL, Liu G, He Y, et al. Ultrasound-guided 7-gauge vacuum-assisted core biopsy: Could it be sufficient for the diagnosis and treatment of intraductal papilloma? Breast J 2019;25:807-12. [Crossref] [PubMed]
- Jain AL, Mullins J, Smith JR, et al. Unusual recurrent metastasizing benign breast papilloma: a case report. J Med Case Rep 2020;14:33. [Crossref] [PubMed]
- Hassan Z, Boulos F, Abbas J, et al. Intracystic papillary carcinoma: clinical presentation, patterns of practice, and oncological outcomes. Breast Cancer Res Treat 2020;182:317-23. [Crossref] [PubMed]
- Zheng YZ, Hu X, Shao ZM. Clinicopathological Characteristics and Survival Outcomes in Invasive Papillary Carcinoma of the Breast: A SEER Population-Based Study. Sci Rep 2016;6:24037. [Crossref] [PubMed]
- Mogal H, Brown DR, Isom S, et al. Intracystic papillary carcinoma of the breast: A SEER database analysis of implications for therapy. Breast 2016;27:87-92. [Crossref] [PubMed]
- Sedano P, Candini D. Do all Cases of Tumorectomy in Breast Cancer need Adjuvant treatments? About therapies in Encapsulated Papillary Carcinomas. Canc Therapy & Oncol Int J 2018;11:555804.
- Zhang J, Zhang T, Wu N, et al. Intracystic papillary carcinoma of the breast: Experience of a major Chinese cancer center. Pathol Res Pract 2018;214:579-85. [Crossref] [PubMed]
- Huang K, Appiah L, Mishra A, et al. Clinicopathologic Characteristics and Prognosis of Invasive Papillary Carcinoma of the Breast. J Surg Res 2021;261:105-12. [Crossref] [PubMed]
- Fakhreddine MH, Haque W, Ahmed A, et al. Prognostic Factors, Treatment, and Outcomes in Early Stage, Invasive Papillary Breast Cancer: A SEER Investigation of Less Aggressive Treatment in a Favorable Histology. Am J Clin Oncol 2018;41:532-7. [Crossref] [PubMed]
- Turashvili G, Brogi E, Morrow M, et al. The 21-gene recurrence score in special histologic subtypes of breast cancer with favourable prognosis. Breast Cancer Res Treat 2017;165:65-76. [Crossref] [PubMed]
- NCCN Clinical Practice Guidelines in Oncology: NCCN Guidelines; 2021 [cited 2021 Aug 23]. Available online: https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf
Cite this article as: Khan M. Treating papillary tumors of the breast—role of adjuvant treatment—a narrative review. Ther Radiol Oncol 2023;7:7.