Successful treatment of locally advanced small-cell carcinoma of the hypopharynx with radiotherapy and cetuximab combination: a case report
Introduction
The occurrence of small-cell carcinoma is rarely reported outside of the lung (1), accounting for only approximately 2.5–5.0% of all cases (2). Among all sites in the head and neck area, the hypopharynx constitutes an exceptionally rare site, whereas the adjacent structure, the larynx, is the most commonly affected area (3). Typically, patients with small-cell carcinoma of the head and neck region present with locally advanced stage (4), and no established guideline or consensus exists regarding the management because of the paucity of the disease. Treatment of hypopharyngeal small-cell carcinoma comprises surgery, radiotherapy (RT), chemotherapy, or their combination, and chemotherapy regimen selection is primarily extrapolated from the treatment experiences of small-cell lung cancer (5). Here, we report the case of an 81-year-old male with locally advanced small-cell carcinoma originating from the pyriform sinus.
Case presentation
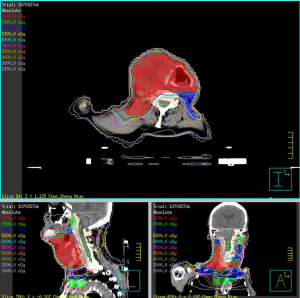
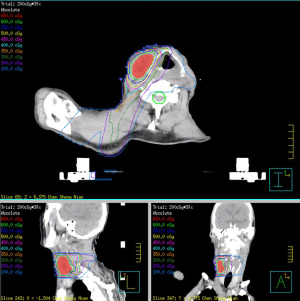
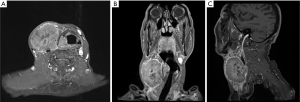
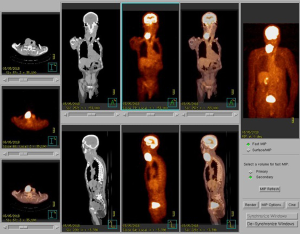
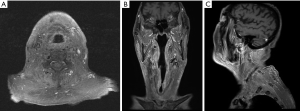
An 81-year-old male presented with an enlarging mass at the right neck for weeks. Physical examination suggested indurated mass (approximately 6 cm in diameter). Laboratory tests were performed, and the results were unremarkable. A fiberscope detected a tumor at the hypopharynx, following which a biopsy of the lesion was performed, with the pathological result revealing small-cell carcinoma (Figure 1). Three days later, using subsequent imaging studies, including magnetic resonance imaging (MRI) (Figure 2) and positron emission tomography (Figure 3), the disease was staged as cT2N3bM0 based on the American Joint Committee on Cancer 8th edition, with an enhanced heterogeneous mass lesion (15 mm × 25 mm × 29 mm) in the right pyriform sinus and confluent lymphadenopathies along the right cervical chain (up to 79 mm), encasing and compressing the right common carotid artery and right internal jugular vein. The patient’s medical history was unremarkable; he was a farmer and an ex-smoker with a 10 pack-year smoking history. Regarding his treatment of choice, considering the disease extension, his performance status, senior age, and his discretion, surgery was not considered. Despite suggesting concurrent chemoradiation (CCRT) using the etoposide and cisplatin (EP) regimen, the patient declined because of fear of treatment toxicity. Then, we advised RT combined with concurrent biotherapy with cetuximab (Bio-RT). Accordingly, we planned RT with 70 Gy in 35 fractions to the hypopharyngeal tumor, lymphadenopathies, and right neck level Ib to V; 63 Gy to the right neck, left neck level II to V, and right supraclavicular fossa; 56 Gy to the left supraclavicular fossa and bilateral infraclavicular fossae (Figure 4). Meanwhile, seven cycles of cetuximab was concurrently applied with RT course, with a loading dose of 600 mg (400 mg/m2) for one cycle followed by a dose of 400 mg (250 mg/m2) for six cycles administered once weekly. An adaptive plan was used because of tumor shrinkage after 18 fractions of RT. After 35 fractions of comprehensive irradiation, a boost dose was administered to the shrunk lymphadenopathy along the right cervical chain with 6 Gy in three fractions (Figure 5). Acute adverse effects included grade 1 dermatitis, mucositis, and dysphagia. After 7-month Bio-RT treatment, complete remission was observed in the follow-up MRI (Figure 6). Notably, there have been no late complications except mild neck stiffness noted over 12 months of follow-up. Aside from reminding the patient of the importance of neck exercise, we also referred him to the specialty of physical medicine and rehabilitation for more suggestion.

Discussion
To date, no established guideline or consensus exists regarding the management of small-cell carcinoma of the hypopharynx because of the paucity of the disease. Nakahira et al. reported two cases with a review of nine additional cases. These eleven cases all presented with cervical lymph node metastases initially, with distant metastases noted in two cases. Most of the cases presented with pyriform sinus involvement, an area of predilection of squamous cell carcinomas. Interestingly, more than half of the patients with small-cell carcinoma of the hypopharynx had tumors which contained mixed elements of small-cell carcinomas and squamous cell carcinomas (5). However, our patient is a case of a pure small-cell carcinoma of the right pyriform sinus. An analysis of the National Cancer Database showed that small-cell carcinomas of the hypopharynx comprises only 4% of all small-cell carcinomas of the head-and-neck area, with those arising from the larynx comprising 35%. Unfortunately, there exists only a combined survival data for small-cell carcinomas of the larynx and hypopharynx. The median overall survival is 19.1 months for locally-advanced small-cell carcinomas of the larynx and hypopharynx, and there was no survival benefit with the addition of surgery to CCRT in locally-advanced small-cell carcinomas of the larynx and hypopharynx (4). A similar choice of systemic chemotherapy regimen using EP is primarily extrapolated from the treatment experiences of small-cell lung cancer (5). Our patient, however, despite being recommended CCRT with such chemotherapy regimen, refused it because of fear of its toxicity. Alternatively, Bio-RT was applied, although we performed no epidermal growth factor receptor staining on the biopsy specimen. Cetuximab has been extensively used as a potent systemic therapy choice in head and neck cancer since the successful Bonner trial (6), although the latest evidence of the De-ESCALaTE HPV trial comparing CCRT versus Bio-RT in human papillomavirus-positive oropharyngeal cancer revealed inferior tumor control when Bio-RT was used, suggesting that cisplatin and RT could be used as the standard of care for HPV-positive low-risk patients who can tolerate cisplatin (7). However, it remains debatable whether our patient is physically fit to undergo CCRT, let alone his reluctance to undergo chemotherapy in the first place. Fortunately, he attained complete remission with Bio-RT. Regarding the RT dosage, although no compelling evidence explains how high the RT dose should be to control the disease, most case reports and series have used a RT dose not lower than 50–60 Gy to promote outcome (3,8).
Regarding small-cell carcinoma of the lung, Auperin meta-analysis established the superiority of prophylactic cranial irradiation (PCI) given to patients in complete remission (9); nevertheless, in patients with small-cell carcinoma of the hypopharynx, it remains a debatable issue. Reportedly, the occurrence of brain metastasis is too high to not give PCI, while some deemed otherwise (10,11). In our case, after attaining complete remission, we did not select PCI considering the uncertainties mentioned above, including his old age, performance status, and his decision to not receive PCI after thoroughly explaining possible benefits and adverse effects.
Small-cell carcinoma of the hypopharynx is a rare and less investigated disease with a poorer prognosis than other carcinomas of the head and neck. Clinically, it shares the same dismal prognosis with those that arise in the lungs (4). Further randomized-controlled trials, although difficult to attain because of the paucity of the disease, are warranted to offer better treatment combination and hopefully augment the survival of patients.
Conclusions
This report demonstrates that the combination of definitive RT and cetuximab could be an effective treatment approach with tolerable treatment-related toxicity in patients with locally advanced small-cell carcinoma of the hypopharynx.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Renner G. Small cell carcinoma of the head and neck: a review. Semin Oncol 2007;34:3-14. [Crossref] [PubMed]
- Remick SC, Hafez GR, Carbone PP. Extrapulmonary small-cell carcinoma. A review of the literature with emphasis on therapy and outcome. Medicine (Baltimore) 1987;66:457-71. [Crossref] [PubMed]
- Lee JH, Jeong JS, Kim SR, et al. Small cell carcinoma of the pyriform sinus successfully treated with concurrent chemo-radiotherapy: A case report. Medicine (Baltimore) 2016;95:e4759 [Crossref] [PubMed]
- Pointer KB, Ko HC, Brower JV, et al. Small cell carcinoma of the head and neck: An analysis of the National Cancer Database. Oral Oncol 2017;69:92-8. [Crossref] [PubMed]
- Nakahira M, Kuba K, Matsumura S, et al. Primary Small Cell Carcinoma of the Hypopharynx: A Report of Two Cases and Review of Nine Additional Cases. Case Rep Otolaryngol 2017;2017:8143145 [Crossref] [PubMed]
- Bonner JA, Harari PM, Giralt J, et al. Radiotherapy plus cetuximab for locoregionally advanced head and neck cancer: 5-year survival data from a phase 3 randomised trial, and relation between cetuximab-induced rash and survival. Lancet Oncol 2010;11:21-8. [Crossref] [PubMed]
- Mehanna H, Robinson M, Hartley A, et al. Radiotherapy plus cisplatin or cetuximab in low-risk human papillomavirus-positive oropharyngeal cancer (De-ESCALaTE HPV): an open-label randomised controlled phase 3 trial. Lancet 2019;393:51-60. [Crossref] [PubMed]
- Sun R, Fairchild A, Debenham B. Small Cell Carcinoma of the Hypopharynx. Cureus 2018;10:e2987 [PubMed]
- Auperin A, Arriagada R, Pignon JP, et al. Prophylactic cranial irradiation for patients with small-cell lung cancer in complete remission. Prophylactic Cranial Irradiation Overview Collaborative Group. N Engl J Med 1999;341:476-84. [Crossref] [PubMed]
- Yazici O, Ozdemir NY, Sendur MA, et al. Current approaches for prophylactic cranial irradiation in extrapulmonary small cell carcinoma. Curr Med Res Opin 2014;30:1327-36. [Crossref] [PubMed]
- Mason M, Giuliani M, Huang SH, et al. Extra-pulmonary small cell carcinoma in the head and neck setting: the role of prophylactic cranial irradiation. Oral Oncol 2015;51:e57-9. [Crossref] [PubMed]
Cite this article as: Huang YH, Chang TH, Lin JB, Liu MT, Pi CP, Huang CC, Hung LC, Chou TW, Tseng PY. Successful treatment of locally advanced small-cell carcinoma of the hypopharynx with radiotherapy and cetuximab combination: a case report. Ther Radiol Oncol 2019;3:27.