Identifying the non-addressed issues in Radiation Oncology—a preliminary opinion collection of radiation oncology community
Introduction
ROs are responsible for the clinical decisions and MPs are responsible for all technological issues that may arise during the process of treatment of a patient by radiotherapy. It is one of the best examples of teamwork in medical science. It is fully understood that for effective functioning, both sub-disciplines need to understand each other very effectively. We tried to understand the lacunae and day-to-day intradepartmental problems faced by our peers. We conducted an exercise of collecting opinion among MPs and ROs. The questions and their response categories were arbitrary and based on the researchers’ personal experience over the years across a numbers of institutions they have worked. We tried to identify the problems with the belief that understanding these lacunae will help us to be more rational in understanding each other’s limitation and will help us to be more realistic. This will eventually improve practical delivery of the treatment and hence possibly enhance patient care.
Methods
Study design
- Observational and cross-sectional, taking opinion of qualified medical physicists and physicians who are working in a Radiation Oncology department.
- Informed consent is not required for such web-based studies, responding to the survey implies consent (all incomplete respondents were excluded from analysis, we considered incomplete responses as withdrawal of consent).
- Method of data collection—via “Survey monkey”, this is a web-based survey system.
- Survey method was not un-anonymous. The opinion collection was open for 2 months, December 2015–January 2016.
Inclusion criteria
- Radiation oncologists working in a cancer center with radiotherapy treatment facilities.
- Medical physicists working in a cancer center with radiotherapy treatment facilities.
Exclusion criteria
- Other coworkers like dosimetrists and radiotherapy technologists.
- Radiation professionals at the authors’ institution to avoid any bias.
A survey titled “Mutual Professional relationship and understanding between Radiation Oncologists and Medical Physicist—A Survey” was conducted over a period of 2 months. The professional survey website Survey monkey was used; the survey website can be used for medical research (1). The email addresses were collected from the professional directories of professional bodies like Association of radiation oncologists of India (AROI), Association of medical physicists of India (AMPI), American society of radiation oncologists (ASTRO), International Atomic Energy Agency (IAEA) booklet and also collected from internet by browsing departmental webpages of many radiation oncology institutions. AROI and AMPI directories represent India, a typical developing country. IAEA hand book was used to collect email addresses of underdeveloped countries like African countries and South America, ASTRO has a worldwide membership representing a global international community, practicing radiation in affluent hospitals worldwide. We used 19 questions via Survey monkey to take opinion. The questions were aimed to collect the opinions of MP and RO on similar situations. Questions 1–5 were meant for collecting background data of the survey respondents; questions 6–19 were targeted towards gathering information on mutual understanding and departmental workflow. The questions and their response categories were arbitrary and based on the researchers’ personal experience over the years of their practice. We decided to make a non-anonymous survey as it maximizes response (2).
Data analysis
Data were compiled and the response to each question was analyzed. The response of MPs and ROs were compared and the difference of opinion for similar questions was noted by simple Chi square test. Subgroup analysis was not done.
Responses of Europe, Australia, North America and Asia were categorized under developed countries and the responses from India and Indian subcontinent, Africa and South America were categorized under developing countries (Q2). In the type of institution categorization only teaching and non-teaching categories were created irrespective of state-owned or private-owned hospitals (Q5). Simple statistical methods were used and percentages, bar charts were derived.
Results
The overall response rate was 19.9% in the MP group and 16.4% in the RO group. The final analysis was done for 176 MPs and 180 ROs. All incomplete responders were omitted as we considered it withdrawal of consent (Table 1).
Table 1
| Summary of mails | MP | RO |
|---|---|---|
| Email sent’ to | 1,404 | 1,836 |
| Opted out | 28 | 89 |
| Total response | 280 (19.94%) | 301 (16.4%) |
| Incomplete/rejected | 104 | 121 |
| For analysis | 176 | 180 |
MP, Medical Physicist; RO, Radiation Oncologist.
Table 2 shows that the respondent group was a matched group and only a significant difference was there when respondents from teaching versus non-teaching facilities were considered.
Table 2
| Categories | MP | RO | P |
|---|---|---|---|
| Country | 0.612 | ||
| Developed | 79 | 76 | |
| Developing | 97 | 104 | |
| Technique used IMRT/IGRT in percentage of cases | 0.458 | ||
| <25 | 27 | 29 | |
| >25 | 19 | 27 | |
| >50 | 130 | 124 | |
| Experience post qualification | 0.18 | ||
| Less than 5 years | 51 | 41 | |
| More than 5 years | 125 | 139 | |
| Nature of institution | 0.012 | ||
| Teaching | 118 | 142 | |
| Non-teaching | 58 | 38 | |
MP, Medical Physicist; RO, Radiation Oncologist; IMRT, intensity modulated radiotherapy; IGRT, image guided radiotherapy.
Radiation oncology workflow (Q: 6–11) (Figures 1,2)
When it comes to grading their peers, ROs were happier with their counterparts and gave them relatively higher grade in their jobs (Q6). It appears that ROs made more mistakes than MPs at the time of placing the contours for planning (Q7). The same percentage of erratum continued even during the plan finalization (Q8). Interestingly enough, MPs pointed out that they had some special peers who act more indecisively than others. More than 52% of MPs believed the doctors give very tight constraints in more than 50% in their prescriptions, but according to the physicians, they rarely complained that the constraints were tight (Q9). About 44% of ROs and 22% of MPs complained that they were not made to understand the planning/clinical result part ever; the physicians however gave their clinical feedback better than the MPs (Q10). About 10% MPs said that a discussion about the choice of treatment modality was not carried out by their counterparts. About 20% of MPs opined that some individual ROs called them to discuss a case when situation arose (Q11). A minimum of 6% of physicians were never consulted during the planning procedure. Interestingly enough, 40% of physicians were consulted frequently during the process of planning (Q11).
When asked about time for planning, only 25% of MPs thought they got adequate time for planning (Q12). About half of ROs (46%) thought that the planning was optimal for most cases and giving more time would only help in less than 25% cases to improve the plan quality (Q12).
Only 30% of MPs thought they got adequate time for QA in 75–100% of times, a reasonable number of them thought that they needed more time for QA (Q13).
About 56% MPs and 38% ROs thought that more physicists were required in the department (Q14). However, most of the people agree that there was enough number of ROs in the departments (Q15). About 50% MPs and 56% ROs thought that a combined planning and contouring station is necessary. The ROs felt it was a bigger necessity than the MPs (Q16).
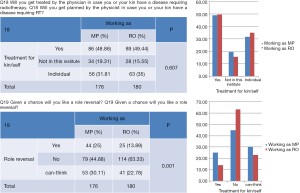
Professional relationship and confidence in the counterpart (Figures 3,4)
The working relationship between two faculties was noted to be good (but not excellent!), professionals across both the faculties were equally comfortable discussing the technical issues (Q17). In the matter of showing confidence in their counterpart, about 50% people were ready to treat their kin in the department (if such situation ever arose). About 30% people relied on one specific counterpart (Q18).
Interestingly, double the percentage of MPs wanted to change their professions (25% vs. 14%). More than half of them (55%) either wanted to shift to RO or stated they might consider it, but among ROs, 63% people had an absolutely negative response to a possible shift to their counterpart’s position (Figure 4; Q19).
Discussion
Response rate of 19% is a reasonable response rate, especially in a web-based survey (which gives 11% lower responses than other survey methods); variable rates from 10–60% are accepted as good response rates (3), but our completed responses available for analysis was about 10% only. The response rates in web-based surveys can be increased by offering incentives to the respondents, we however do not have the requisite funds for the same. We believe that if further studies are conducted in this direction by similar web-based surveys, the issue of incentives should be best addressed by professional bodies like ASTRO and AROI. The percentage of response categorization is quite arbitrary and based on the authors’ own subjective opinion and experience. The survey questions were undoubtedly arbitrary, but considering the day-to-day experience, the response categorization had to be practical (for example, we cannot expect the contouring revision to be more than 20% in any case from our clinical experience, so we have put it like 5%, 10%, and 20%). The response rates for individual questions were categorized for 6 months with mutual discussions by the authors, and it was validated with our peers. As no study has ever addressed such an issue, we had no prior data to fall back on. The response categories are not fixed because the authors estimate it to be different for different questions. Hence this study can be considered a preliminary project in this direction. However the study proves that there are some problems that need to be recognized and need attention to improve the working relationship.
We decided it may be more reasonable to identify the problems and bring them forward before the community of radiation professionals. The radiation oncology professionals practising in different communities under different scenarios should try to identify the relevant problems in their own way and address them accordingly to regional demands.
The study was a first attempt to identify and pinpoint the problems amongst closely aligned professionals (the problems that we know to exist but rarely talked about). Considering it to be a sensitive issue, any region-based survey was not attempted. The problems are not specific to any community or region but to the whole world and this fact was well appreciated from the results of response that we got even from North America and Europe.
The physician has the liberty to think over his contours even after finalizing them and also the right to modify and request for a re-plan during the final phase of planning approval and even at a later state if a justifiable reason exists.
Medical physicists should have a greater say in the matter of time given for planning and QA, and they should have the right to decide when they will be ready with a final plan suitable for treatment delivery. What appears from the survey is that although the physicians think the plans cannot be improved much, the MPs feel they the plan can be improved given more time. It means that if more time is given, the physicians may get better plans than they are actually expecting.
At the same time, many patients requiring early start of treatment should be allowed concessions. The medical physicists are probably less adequately staffed in many centres; this issue should be resolved if it is expected that the departments run seamlessly. ROs feel a greater need of combined contouring and planning room. This is probably due to increased need of technical assistance in new contouring stations. A combined contouring and planning station is possibly needed; this apart from solving many technical issues will help the community to gain in terms of professional knowledge.
However the technical errors can be minimized with the use of more training, consciousness and departmental protocols and optimal communication. Communication between the colleagues is an essential skill for teamwork to radiation treatment administration (4). Optimal communication among the team members can be significantly improved by training. Specific training modules need to be developed based on department-specific requirements. The article by Kannan et al. has pointed out that with increased expansion of treatment facilities and technologies, we need to give more attention to training our professionals (5). Treatment planning conferences and Chart round involving all the stakeholders in the Radiation oncology family can greatly help (6,7).
With 80% of the professionals ready to get their kin treated in the same institute (by any or a particular expert) it is implied that our community has excellent confidence in the work that their peers do.
The last question about crossover to the other side was to see if people think the job of their counterpart was more attractive. We found that a significant number of MPs are willing to crossover rather than ROs. We came across one such example in Europe and United States (8,9).
Limitations
The main limitation of the above study is its small sample size. The survey was conducted on a voluntary basis, hence the response rate was low. The opinion collected here may not be the true representation of the whole radiation oncology community and region-specific surveys may have been a better pattern of study. The response categorization for different questions are also not uniform that makes the survey rather more qualitative than quantitative, making strict statistical derivations rather difficult. Besides recall bias in such self-reporting qualitative study is a major limitation.
Conclusions
There are issues within the workers of radiation health care professionals that need to be identified. The above study is very innovative but just an preliminary step in this direction. This task can be best taken up by professional bodies like ASTRO or AROI. The areas of lacunae should be identified and corrective measures should be taken; that will ultimately transform the workflow and patient care in a better direction.
Just a few suggestions:
- The ROs should try to avoid contour change for technical reasons, however we think that changes of contours during planning or sometimes after giving for final plans is justifiable from some clinical points. The physician has the liberty to change or think in the best interest of the patient. Our opinion is that the physician should revisit a contour after finalizing it. A peer review can solve most of the problems.
- Our peers who face technical difficulties in dealing with the modern planning process should be technically supported.
- Possibly the time of planning should be flexible and the physicist should ask for more time if a better plan can be made.
- There needs to be a common planning and contouring station so that our peers can get immediate help when they feel from their counterparts. May be this will improve training of the residents and also improve the professional relationship from good to excellent.
Supplementary
Mutual Professional relationship and understanding between Radiation Oncologists and Medical Physicist—a survey
Questions 1–5: Respondents profile
- You are a
- Medical Physicist
- Radiation Oncologist
- Dosimetrist
- You work at
- Europe
- Australia
- North America
- Indian Subcontinent
- Asia
- Africa
- South America
- Do you routinely perform 3DCRT/IMRT/IGRT/VMAT/Rapidarc?
- Less than 25% of my cases
- More than 25% of My cases
- More than 50% of my cases
- How many years are you post Qualification as a Medical physicist/Radiation Oncologist?
- Less than 5 years
- More than 5 years
- Which Radiotherapy institute do you work?
- Govt/State Sponsored centre with teaching facilities (MD/FRCR/MSc/Dphys)
- Govt/State Sponsored centre without teaching facilities
- Private Hospital with teaching facilities
- Private Hospital without teaching facilities
Medical Physicist
- Do you like the contours from the planning point of view?
- Comfortable with 100–75% of them
- Comfortable with 75–50% of them
- Comfortable with 50–25% of them
- Comfortable with 25–0% of them
- How many times you need to change contours after they are pushed for planning for technical reasons (organs overlap, wrong nomenclature, wrong colour code)?
- Less than 0–5% time
- More than 5–10% time
- More than 10–20% times
- It is Physician specific
- How many times the physician changes contours during plan evaluation
- Less than 5% times
- More than 5% times
- More than 10% times
- It is Physician specific
- Does your physician give very tight constraints?
- 100–75% of times
- 75–50% times
- 50–25% times
- Less than 25% time
- It is physician specific
- Does your physician give feedback related to planning (complications/cure) when patients come for FU after
- Never
- Less than 10% times
- 10–20% times
- More than 20% time
- There are specific physicians who give feedbacks
- How often your physician calls you to discuss a case (even by phone) before taking for treatment
- Never
- Less than 5% times
- 5–10% times
- 10–20% times
- There are specific physicians who call
- Do you get adequate time for planning
- 100–75% of times
- 75–50% times
- 50–25% times
- Less than 25% time
- Do you get adequate time for QA?
- 100–75% of times
- 75–50% times
- 50–25% times
- Less than 25% time
- It is physician specific
- Do you think the Physics department is understaffed?
- Yes
- No
- Do you think physician department is understaffed?
- Yes
- No
- Do you think a combined planning and contouring station will be better than separate room
- Never
- Must
- Don’t Know
- How much comfortable are you with your Oncologist about discussing technical and planning issues.
- Comfortable with 100–75% of them
- Comfortable with 75–50% of them
- Comfortable with 50–25% of them
- Comfortable with 25–0% of them
- Will you get treated by the physician in case you or your kin have a disease requiring RT.
- Yes
- No
- By a Specific Physician
- Given a chance will you like a role reversal?
- Yes
- No
- Can think
Radiation Oncologist
- Do you like the plans from the clinical point of view?
- Comfortable with 100–75% of them
- Comfortable with 75–50% of them
- Comfortable with 50–25% of them
- Comfortable with 25–0% of them
- How many times you need to change plans, after they are pushed for treatment technical reasons (wrong DRR/not deliverable MU, Others).
- Less than 0–5% time
- More than 5–10% time
- More than 10–20% times
- It is Physician specific
- How many times you have to relax constrains for finalizing the plans?
- Less than 5% times
- More than 5% times
- More than 10% times
- It is Physician specific
- Do your physicist complains of very tight constraints?
- 100–75% of times
- 75–50% times
- 50–25% times
- Less than 25% time
- It is physician specific
- Does your physicist make you understand the technical issues while explaining a plan?
- Never
- Less than 10% times
- 10–20% times
- More than 20% time
- There are specific physicians who give feedbacks
- How often your physicist calls you to discuss a case (even by phone) before showing a final plan?
- Never
- Less than 5% times
- 5–10% times
- 10–20% times
- There are specific physicians who call
- Do you think the plan can be improved with more time?
- 100–75% of times
- 75–50% times
- 50–25% times
- Less than 25% time
- Does the physicist get adequate time for QA?
- 100–75% of times.
- 75–50% times
- 50–25% times.
- Less than 25% time.
- It is physicist specific
- Do you think the Physics department is understaffed?
- Yes
- No
- Do you think physician department is understaffed?
- Yes
- No
- Do you think a combined planning and contouring station will be better than separate room.
- Never
- Must
- Don’t know
- How much comfortable are you with your physicist about discussing technical and planning issues
- Comfortable with 100–75% of them
- Comfortable with 75–50% of them
- Comfortable with 50–25% of them
- Comfortable with 25–0% of them
- Will you get planned by the physicist in case you or your kin have a disease requiring RT
- Yes
- No
- By a Specific Physicist
- Given a chance will you like a role reversal?
- Yes
- No
- Can think
Questions 1–5: Respondents profile
- You are a
- Medical Physicist
- Radiation Oncologist
- Dosimetrist
- You work at
- Europe
- Australia
- North America
- Indian Subcontinent
- Asia
- Africa
- South America
- Do you routinely perform 3DCRT/IMRT/IGRT/VMAT/Rapidarc?
- Less than 25% of my cases
- More than 25% of My cases
- More than 50% of my cases
- How many years are you post Qualification as a Medical physicist/Radiation Oncologist?
- Less than 5 years
- More than 5 years
- Which Radiotherapy institute do you work?
- Govt/State Sponsored centre with teaching facilities (MD/FRCR/MSc/Dphys)
- Govt/State Sponsored centre without teaching facilities
- Private Hospital with teaching facilities
- Private Hospital without teaching facilities
Medical Physicist
- Do you like the contours from the planning point of view?
- Comfortable with 100–75% of them
- Comfortable with 75–50% of them
- Comfortable with 50–25% of them
- Comfortable with 25–0% of them
- How many times you need to change contours after they are pushed for planning for technical reasons (organs overlap, wrong nomenclature, wrong colour code)?
- Less than 0–5% time
- More than 5–10% time
- More than 10–20% times
- It is Physician specific
- How many times the physician changes contours during plan evaluation
- Less than 5% times
- More than 5% times
- More than 10% times
- It is Physician specific
- Does your physician give very tight constraints?
- 100–75% of times
- 75–50% times
- 50–25% times
- Less than 25% time
- It is physician specific
- Does your physician give feedback related to planning (complications/cure) when patients come for FU after
- Never
- Less than 10% times
- 10–20% times
- More than 20% time
- There are specific physicians who give feedbacks
- How often your physician calls you to discuss a case (even by phone) before taking for treatment
- Never
- Less than 5% times
- 5–10% times
- 10–20% times
- There are specific physicians who call
- Do you get adequate time for planning
- 100–75% of times
- 75–50% times
- 50–25% times
- Less than 25% time
- Do you get adequate time for QA?
- 100–75% of times
- 75–50% times
- 50–25% times
- Less than 25% time
- It is physician specific
- Do you think the Physics department is understaffed?
- Yes
- No
- Do you think physician department is understaffed?
- Yes
- No
- Do you think a combined planning and contouring station will be better than separate room
- Never
- Must
- Don’t Know
- How much comfortable are you with your Oncologist about discussing technical and planning issues.
- Comfortable with 100–75% of them
- Comfortable with 75–50% of them
- Comfortable with 50–25% of them
- Comfortable with 25–0% of them
- Will you get treated by the physician in case you or your kin have a disease requiring RT.
- Yes
- No
- By a Specific Physician
- Given a chance will you like a role reversal?
- Yes
- No
- Can think
Radiation Oncologist
- Do you like the plans from the clinical point of view?
- Comfortable with 100–75% of them
- Comfortable with 75–50% of them
- Comfortable with 50–25% of them
- Comfortable with 25–0% of them
- How many times you need to change plans, after they are pushed for treatment technical reasons (wrong DRR/not deliverable MU, Others).
- Less than 0–5% time
- More than 5–10% time
- More than 10–20% times
- It is Physician specific
- How many times you have to relax constrains for finalizing the plans?
- Less than 5% times
- More than 5% times
- More than 10% times
- It is Physician specific
- Do your physicist complains of very tight constraints?
- 100–75% of times
- 75–50% times
- 50–25% times
- Less than 25% time
- It is physician specific
- Does your physicist make you understand the technical issues while explaining a plan?
- Never
- Less than 10% times
- 10–20% times
- More than 20% time
- There are specific physicians who give feedbacks
- How often your physicist calls you to discuss a case (even by phone) before showing a final plan?
- Never
- Less than 5% times
- 5–10% times
- 10–20% times
- There are specific physicians who call
- Do you think the plan can be improved with more time?
- 100–75% of times
- 75–50% times
- 50–25% times
- Less than 25% time
- Does the physicist get adequate time for QA?
- 100–75% of times.
- 75–50% times
- 50–25% times.
- Less than 25% time.
- It is physicist specific
- Do you think the Physics department is understaffed?
- Yes
- No
- Do you think physician department is understaffed?
- Yes
- No
- Do you think a combined planning and contouring station will be better than separate room.
- Never
- Must
- Don’t know
- How much comfortable are you with your physicist about discussing technical and planning issues
- Comfortable with 100–75% of them
- Comfortable with 75–50% of them
- Comfortable with 50–25% of them
- Comfortable with 25–0% of them
- Will you get planned by the physicist in case you or your kin have a disease requiring RT
- Yes
- No
- By a Specific Physicist
- Given a chance will you like a role reversal?
- Yes
- No
- Can think
Acknowledgments
All peers who helped to complete the study by sending response to our survey.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Hiroaki Kumada and Yi-Wei Chen) for the series “Boron Neutron Capture Therapy” published in Therapeutic Radiology and Oncology. The article has undergone external peer review.
Conflicts of Interest: The series “Boron Neutron Capture Therapy” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Informed consent is not required for such web-based studies, responding to the survey implies consent (all incomplete respondents were excluded from analysis, we considered incomplete responses as withdrawal of consent).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
-
SurveyMonkey - Wijnen K, Vermeir I, Kenhove PV. The relationship between topic involvement, topic sensitivity, and two motivational factors, as response inducements in a mail survey context. In: Petrieff LO, Miller RV. editors. Public Opinion Research Focus. Nova Science Publishers, 2008:61-86.
- What is an acceptable survey response rate? Available online: http://socialnorms.org/what-is-an-acceptable-survey-response-rate/
- Gibon AS, Merckaert I, Liénard A, et al. Is it possible to improve radiotherapy team members' communication skills? A randomized study assessing the efficacy of a 38-h communication skills training program. Radiother Oncol 2013;109:170-7. [Crossref] [PubMed]
- Kannan V, Bajpai R. Conforming Modern Radiation Oncology Facilities to the Irregular Contours of the Vast and Varied Nation of India. Int J Radiat Oncol Biol Phys 2016;94:645-51. [Crossref] [PubMed]
- Duggar WN, Bhandari R, Yang CC, et al. Group consensus peer review in radiation oncology: commitment to quality. Radiat Oncol 2018;13:55. [Crossref] [PubMed]
- Brammer CV, Pettit L, Allerton R, et al. Impact of the introduction of weekly radiotherapy quality assurance meetings at one UK cancer centre. Br J Radiol 2014;87:20140422 [Crossref] [PubMed]
-
My Journey from Physicist to Physician - Available online: https://www.heidelberg-university-hospital.com/fileadmin/CV/Debus_CV.pdf
Cite this article as: Banerjee S, Kataria T, Goyal S, Bisht SS, Gupta D, Basu T, Abhishek A, Narang K, Tayal M, Ali I, Karthick KP, Thiyagarajan R. Identifying the non-addressed issues in Radiation Oncology—a preliminary opinion collection of radiation oncology community. Ther Radiol Oncol 2018;2:52.